Achieving Optimal Starts Across the Southeast
Kidney disease has a disproportionate impact on the southeastern U.S., but Interwell Health is working with nephrologists to improve outcomes for patients living in the region.
Kidney disease has a disproportionate impact on the southeastern U.S. The area has one of the highest rates of end-stage kidney disease (ESKD) and one of the lowest rates of kidney transplants1. Comorbidities like diabetes and hypertension are also extremely common.
To help change the trends, Interwell Health is working with nephrologists to improve outcomes for patients living in the region.
One focus: Prioritizing optimal starts.
By ensuring a planned transition to dialysis or transplant, known as an “optimal start,” costly hospital stays can be avoided, complications can be reduced, and quality of life can be enhanced.
"For a small practice like ours, it’s difficult to do all of this on our own. Working with Interwell has helped us achieve good outcomes like optimal starts for our patients."
Meaningful results
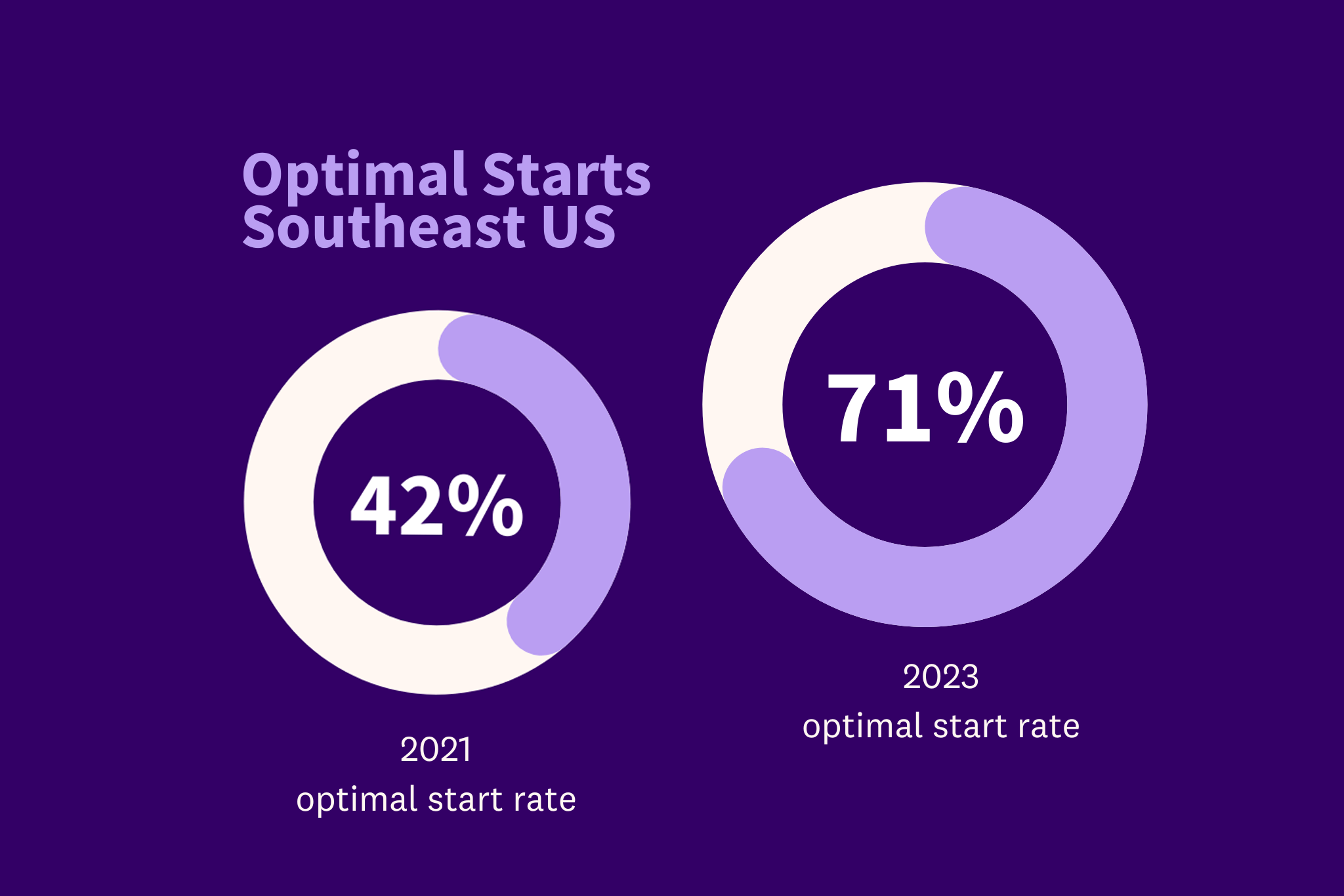
Nephrology practices in the southeast saw significant improvements in their optimal start rates. Optimal start rates rose from 42 percent in 2021 to 71 percent in 2023 for patients in a government value-based care program – representing a 69 percent increase over two years.
Research roundup: the toll of unplanned starts
While optimal starts benefit patients and healthcare systems, unplanned starts result in worse outcomes and higher costs. Here are a few findings:
- Unplanned starts increase medical costs. A retrospective study of 495 patients found that when compared with optimal starts, patients with an unplanned start incurred an additional $16,565 of medical costs in the first 12 months of dialysis.3
- Unplanned starts increase the risk of hospitalization after dialysis initiation. The same study found that admissions per 1,000 in the first 12 months of dialysis increased from 291 per 1,000 for patients with an optimal start to 853 per 1,000 for those with an unplanned start.3
- Unplanned starts lead to worse patient outcomes. Additional studies have confirmed that patients who experience unplanned starts have a higher risk of catheter-related bloodstream infection, mortality, and lower quality of life.4
Empowering nephrologists
We empower nephrologists to prepare patients for ESKD by identifying high-risk patients, educating them and their families proactively, helping them make appropriate choices, and then successfully coordinating their transition to dialysis or transplantation as kidney function declines. Here are three essential components of our approach:
1. Predictive analytics
To predict which patients are likely to decline – meaning they might soon progress to ESKD – we use a powerful analytics engine that considers claims data and other patient factors.
Our population health team develops insights that are shared directly with nephrology practices and care teams. This information is used to identify -- and provide – personalized care at the right time.
Annie Silverman, senior director of population health programs, detailed how these analytics guide patient interventions:
“Interwell leverages our robust analytics to inform physicians about their patient population capturing the full patient journey. The analytics encompass aspects such as readmission rates and discharge patterns, among other factors. This comprehensive picture of the data helps us educate and partner with our physicians on areas of potential opportunities to improve care delivery.”
2. Proactive education
Proactive patient education is an essential component of optimal starts. We provide practices within our Interwell Provider Network with the opportunity to access an innovative kidney disease education suite designed by nephrologists, for nephrologists.
Our program combines video content, one-on-one physician educator-patient sessions, and printed materials to help patients make informed decisions about their care.
3. Connected, coordinated care
Interwell deploys multidisciplinary care teams — made up of coordinators, nurses, social workers, and renal dietitians — to help patients make lifestyle changes that can slow progression to kidney failure, giving them more time to make informed decisions about the dialysis modality that’s best for them.
Our embedded renal care coordinators work directly with nephrologists and patients to close gaps in communication and care. Before a patient transitions to dialysis, renal care coordinators help them understand what to expect. They can assist with steps like modality selection and training, surgical consults, access placement, and transplant coordination.

A collaborative partnership
Shaun Conlon, MD, an Interwell-affiliated nephrologist at Atlanta Nephrology Associates in Georgia, has seen the benefits of our approach firsthand. His practice partnered with Interwell in 2021 and they have been working with an embedded renal care coordinator for three years.
“It’s a collaborative relationship between the coordinator and the nephrologist,” he explained.
“Our renal care coordinator follows our patients and knows what things need to be accomplished in their care journey. If a patient needs education, she’ll let me know so we can talk about that. If they’ve selected a dialysis modality, she’ll help me connect them to a surgeon.”
The care coordinator also closes communication gaps and ensures continuity of care for patients transitioning to ESKD. “She helps patients through the process, whether that’s seeing a surgeon to get evaluated for a catheter or a fistula placement. And if a patient misses an appointment, she can help them reschedule,” he said.
The result of all this support and coordination? Better outcomes and quality of care. “For a small practice like ours, it’s difficult to do all of this on our own,” Conlon said. “Working with Interwell has helped us achieve good outcomes like optimal starts for our patients.”
Notes:
1. USRDS Data.
2. Kidney Transplant Access in the Southeast: View from the Bottom. American Journal of Transplantation.
3. Dialysis Costs for a Health System Participating in Value-Based Care. American Journal of Managed Care.
4. Measuring Quality in Kidney Care: An Evaluation of Existing Quality Metrics and Approach to Facilitating Improvements in Care Delivery. Journal of the American Society of Nephrology.